Lawyers helping elders
and their families,
through legal problems
which come with ageing

Lawyers helping elders and their families, through legal problems which come with ageing
Elderlaw Aged
Care Contract
Ten things you need to know
about your aged care contract

Click here
Elderlaw
Resources
Articles, seminars & media

Access your library
Elderlaw
Links
A selection of the best
resources to get you started

Have a look now
Welcome to Elderlaw ‘The Law Firm’
Our law firm ‘Elderlaw, aims to inform and assist those of us in the Australian
community who are elders or whose parents, close relatives, friends, siblings or
neighbours are elders and who have an elder law problem.
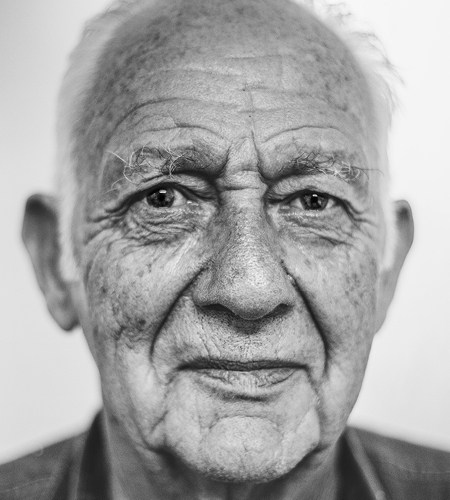
Who is an Elder and what is Elder Law?
An elder is a person whose experience of life provides them with the authority to command respect from others or to whom other defer for that reason.
Elder law in Australia is a developing and increasingly popular part of the practice of law. Elder law also involves other professionals including medical practitioners and aged care nurses, financial planners, accountants and students in nursing, law and medicine.
Elder Law is also about viewing the law through the prism and experience of ageing. There are many life events associated with ageing which require or involve attention from a legal perspective. They include:
- Financial disputes with business, banks, family and friends;
- Delegation of decision-making capacity including financial,
property, healthcare and accommodation decisions; - Financial issues such as social security, residential aged
care charges and fees, taxation, retirement planning, estate
& business succession planning & superannuation; - Life and death issues including termination, refusal and
withdrawal of medical treatment; - Powers of attorney;
- Making wills;
- Challenging wills;
Our People

Rodney Lewis
Senior Solicitor
Author of the text: Elder Law in Australia, 2nd edn, Lexis Nexis, Sydney 2012; has practised in Elder Law since 1999 and longer, in wills and estates; has been delivering elder law education by way of talks and seminars to the legal profession and to the community, in elder law, for many years.

Nicole Louvris
Legal Support
An experienced legal support assistant who is involved in client work production, file and systems management.

Teigan Hutchison
Solicitor
After her admission to the Supreme Court in February 2023, Teigan has assisted with a variety of legal matters, including family law, wills, debt recovery, and commercial litigation.
Teigan has become a vital supporting role in our various matters and disputes, demonstrating punctuality, problem-solving abilities, and commitment to her ongoing professional learning and development.

Sanchit Paul
Lawyer
Sanchit joined our team in 2023 through the placement program. After being admitted to the NSW Supreme Court, he transitioned into the graduate lawyer position.
Sanchit assists in various legal areas including commercial, corporate, litigation, wills and probate. He values trust and empathy, understanding that every client’s situation is unique and requires a tailored solution.
Stay in touch
Receive our newsletter